Français / Español / 简体中文 / русский / العربية / 日本語
© 2025 World Federation of Hemophilia
Platelets are small disc-shaped cells that circulate in the blood. They play an important role in the formation of blood clots to help stop bleeding and in the repair of damaged blood vessels.
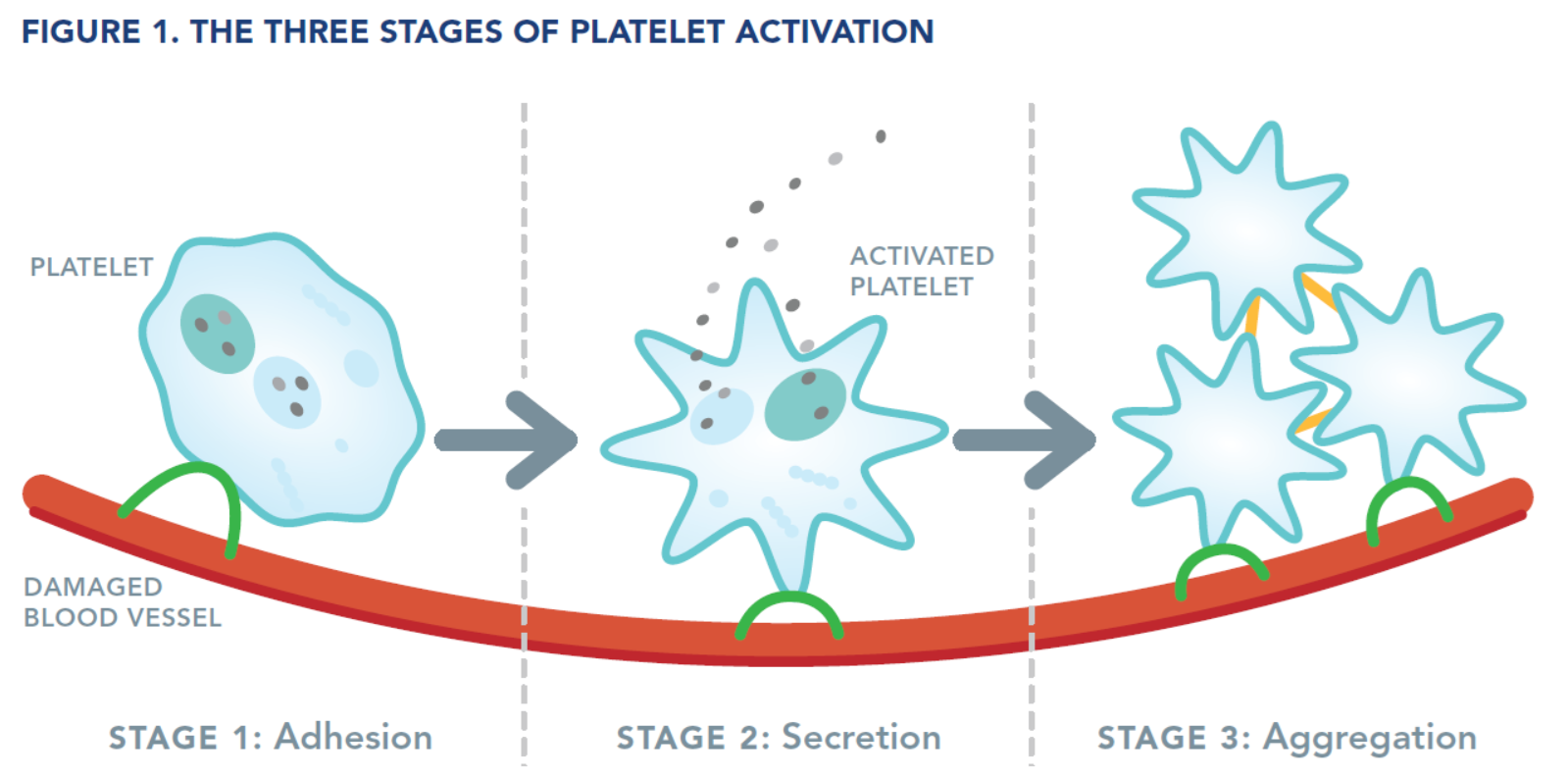
When a blood vessel is injured, platelets begin the process to stop the bleeding by forming what is called a platelet plug. This happens in three stages (see Figure 1):
As the platelet plug is forming, proteins called clotting factors are also recruited to the site of injury. These clotting factors work together on the surface of the platelets to strengthen the platelet plug by forming a mesh called a fibrin clot.
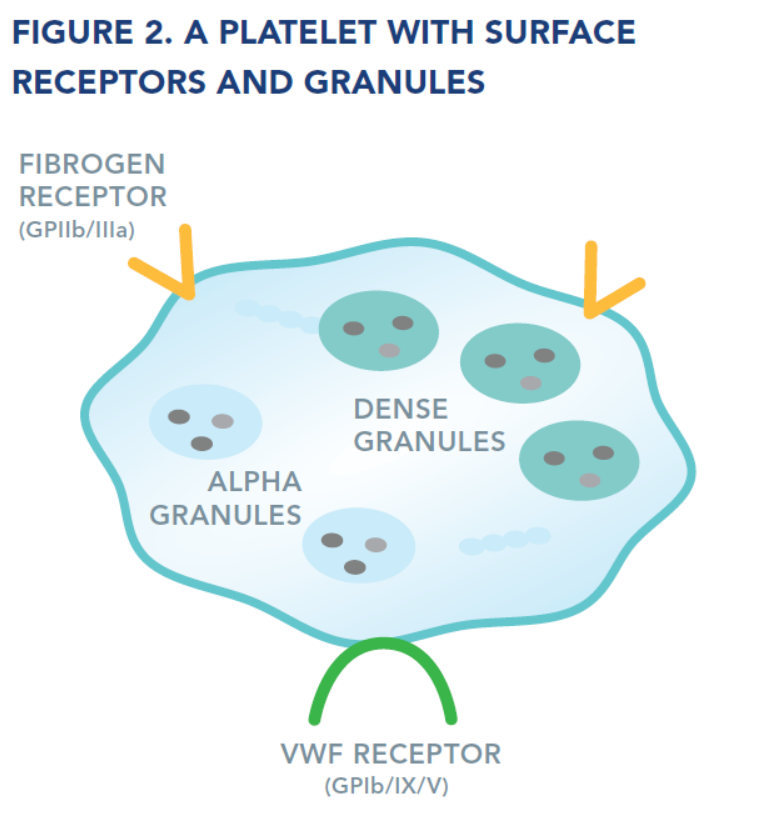
Platelets have several components, such as receptors on their surface and internal granules, that all contribute to clot formation.
Receptors
Receptors are proteins on the surface of the platelets that help the platelet interact with, and respond to, chemicals, proteins, or other blood cells.
Granules
Granules are small packets inside the platelets where proteins and other chemicals are stored. The contents of the granules are released from the platelet during the secretion phase of activation. These molecules act as signals to recruit more platelets and other cells to the site of injury to stop the bleeding.
There are two types of granules: alpha granules and dense granules. The contents differ between the alpha and the dense granules, and they work in different ways to recruit more platelets, activate the clotting factors, and stop the bleeding.
Platelet function disorders are conditions in which the platelets do not work the way they should. If the platelet plug does not form properly, bleeding can continue for longer than normal. People with platelet function disorders tend to bruise or bleed more easily than normal. Platelet function disorders can be caused by a problem with one of the receptors, with the granules, or with activation processes inside the platelets, and may not be associated with a low platelet count.
There are inherited (i.e., passed down from parent to child) and acquired platelet function disorders. This booklet addresses inherited platelet function disorders.
Bernard-Soulier syndrome is an inherited platelet function disorder caused by an abnormality in the receptor for von Willebrand factor (VWF, see Figure 2). This receptor is also called Glycoprotein (GP) Ib/IX/V. Receptors are proteins on the surface of the platelets that help them interact with, and respond to, other blood cells or substances. Since the VWF receptor is absent or does not work properly, the platelets cannot bind to VWF and do not stick to the injured blood vessel wall the way they should. As a result, the platelet plug does not form normally.
Bernard-Soulier syndrome is an autosomal recessive disorder, meaning that both parents carry a genetic change (even though they themselves do not usually have the disorder, they may have mild bleeding symptoms), and pass this changed gene on to their child. Bernard-Soulier syndrome affects both males and females.
The symptoms of Bernard-Soulier syndrome vary from one individual to another. Signs of the disorder are usually first noticed during childhood.
People with Bernard-Soulier syndrome may experience:
Bernard-Soulier syndrome may cause more problems for women than men in early adulthood because of the risk of bleeding associated with menstruation and childbirth.
No single test can diagnose all platelet function disorders. The diagnosis of Bernard-Soulier syndrome requires a careful medical history and a series of laboratory tests that should be performed by a specialist at a bleeding disorder treatment centre.
In people with Bernard-Soulier syndrome:
Note: Some tests are not available in all centres.
Bernard-Soulier syndrome is sometimes misdiagnosed as immune thrombocytopenia (ITP), an acquired platelet disorder in which the platelet count is low.
Most people with Bernard-Soulier syndrome need treatment before surgical procedures (including dental work) or after injury or accidents. Some people will need treatment for severe nose bleeds or other bleeding symptoms, such as heavy menstrual bleeding.
When needed, Bernard-Soulier syndrome may be treated with:
See Treatment Products for more details.
People with Bernard-Soulier syndrome should not take aspirin (acetylsalicylic acid), other nonsteroidal anti-inflammatory drugs (such as ibuprofen and naproxen), or blood thinners (anticoagulants), as these can worsen bleeding symptoms.
Glanzmann thrombasthenia is an inherited platelet function disorder caused by an abnormality in the receptor for fibrinogen (also called GPIIb/IIIa, see Figure 2). Receptors are proteins on the surface of the platelets that help the platelet interact with, and respond to, other blood cells or substances. Since the fibrinogen receptor is absent or does not work properly, the platelets do not stick to each other at the site of injury. As a result, the platelet plug does not form normally.
Glanzmann thrombasthenia is an autosomal recessive disorder, meaning that both parents carry a genetic change (even though they themselves do not usually have the disorder), and pass this changed gene on to their child. Glanzmann thrombasthenia affects both males and females.
Symptoms of Glanzmann thrombasthenia vary from one individual to another and range from mild to potentially life-threatening bleeding. Signs of the disorder are usually first noticed during childhood.
People with Glanzmann thrombasthenia may experience:
Glanzmann thrombasthenia may cause more problems for women than men in early adulthood because of the risk of bleeding associated with menstruation and childbirth.
No single test can diagnose all platelet function disorders. The diagnosis of Glanzmann thrombasthenia requires a careful medical history and a series of laboratory tests that should be performed by a specialist at a bleeding disorder treatment centre.
In people with Glanzmann thrombasthenia:
Note: Some tests are not available in all centres.
Most people with Glanzmann thrombasthenia need treatment before surgical procedures (including dental work) or after injury or accidents. Some people will need treatment for severe nose bleeds or other bleeding.
When needed, Glanzmann thrombasthenia may be treated with:
See Treatment Products for more details.
People with Glanzmann thrombasthenia should not take aspirin (acetylsalicylic acid), other nonsteroidal anti-inflammatory drugs (such as ibuprofen and naproxen), or blood thinners (anticoagulants), as these can worsen bleeding symptoms.
Platelet granules are small packets inside the platelets in which proteins and other chemicals are stored. The contents of the granules are released during the secretion phase of platelet activation (see Figure 1), acting as chemical signals to recruit more platelets and other cells to the site of injury to stop the bleeding. There are two types of granules: alpha granules and dense granules (see Figure 2).
Platelet granule disorders are a diverse group of inherited disorders. Some are caused by an absence of granules or their contents, but the most common are caused by a failure of the platelets to release their granule contents into the bloodstream.
The way that platelet granule disorders are inherited (i.e., passed down from parent to child) is less consistent than for other types of platelet disorders and varies from one individual to the next.
Symptoms of platelet granule disorders vary from one individual to the next.
People with granule disorders may experience:
No single test can diagnose all platelet function disorders. The diagnosis of platelet granule disorders requires a careful medical history and a series of laboratory tests that should be performed by a specialist at a bleeding disorder treatment centre.
In people with granule disorders:
Many people with platelet granule disorders need treatment before surgical procedures (including dental work) or after injury or accidents.
When needed, people with platelet granule disorders may be treated with:
See Treatment Products for more details.
People with platelet granule disorders should not take aspirin (acetylsalicylic acid), other nonsteroidal anti-inflammatory drugs (such as ibuprofen and naproxen), or blood thinners (anticoagulants), as these can worsen bleeding symptoms, unless prescribed for a specific reason by a physician familiar with their disorder.
There are many other types of inherited platelet function disorders, however the principles of management remain the same. Some platelet function disorders may be associated with other blood disorders. Investigations for these other blood disorders may be indicated in particular cases.
All treatments may have side effects. People with inherited platelet disorders should talk to their health care provider about possible side effects before taking any medication. For more information about medicines and herbal remedies that should not be used by people with bleeding disorders, please ask your health care provider. In rare circumstances, these medications may have to be considered for the management of other medical conditions. Their use should be discussed with the physician who leads on the management of the platelet disorder.
The antifibrinolytic drugs tranexamic acid and aminocaproic acid are used to prevent the breakdown of a clot in certain parts of the body, such as the nose, mouth, bladder, and uterus. These medications are useful in many situations, such as during dental work, but are not appropriate for genitourinary bleeding. They can be used to decrease bleeding during and after some types of surgery. Antifibrinolytic drugs are also used to manage heavy menstrual bleeding. They can be applied directly to sites of bleeding in the nose or mouth. They can also be given by mouth or by injection.
Recombinant factor VIIa is an activated clotting factor that is given by injection. It can be effective to treat bleeding in some people with Glanzmann thrombasthenia or Bernard-Soulier syndrome and to prevent bleeding prior to surgery. It is particularly useful as an alternative to platelet transfusion to prevent people from developing antibodies to platelets, or to provide treatment in cases where antibodies have already developed (see Platelet Transfusions, below). Recombinant factor VIIa is made in a laboratory and not from human plasma.
Desmopressin (DDAVP) is a synthetic hormone that can help control bleeding in an emergency or during surgery. It can be injected intravenously or under the skin (subcutaneously), or given as a nasal spray. Desmopressin does not work for every platelet disorder or individual. After receiving desmopressin, it is important to restrict fluid intake for the following 24 hours. Desmopressin is not usually given to people with an increased risk of cardiovascular disease.
Fibrin sealants (also called fibrin glue) are available in some countries. They can be used to treat external wounds and during dental work, such as tooth extraction. Fibrin sealants are applied directly to the bleeding site.
Hormonal suppressive therapy (birth control medications) and the levonorgestrel-releasing intrauterine device/system can be used by women who do not wish to conceive to help manage heavy menstrual bleeding.
Iron replacement is required to treat anemia, or iron deficiency without anemia, caused by excessive or prolonged bleeding. Iron replacement can be given by mouth or by injection. People who bleed frequently should have blood tests to monitor for anemia and/or low iron.
Platelet transfusions may be necessary to treat severe or uncontrolled bleeding, or to prevent bleeding during or after surgery. Although platelet transfusions may be very effective, they are avoided whenever possible because some people may develop antibodies to the transfused platelets, making future transfusions less effective. In some countries, platelets are selected to reduce the risk of antibody development, referred to as human leukocyte antigen (HLA) selected platelets.
Women with inherited platelet function disorders may experience more symptoms than men because of the risk of bleeding associated with menstruation and childbirth. Girls may experience heavy bleeding when they begin to menstruate.
Women with inherited platelet function disorders may have heavier and/or longer menstrual flow that could lead to iron deficiency (low levels of iron, which results in weakness and fatigue) and/or anemia (low levels of red blood cells).
Women with inherited platelet function disorders should receive genetic counseling about the risks of having an affected child well in advance of a planned pregnancy and should be seen by an obstetrician as soon as they suspect they are pregnant. The obstetrician should work closely with the staff of the bleeding disorder treatment centre to provide the best care during pregnancy and childbirth, and to minimize potential complications for both the mother and newborn.
The main risk related to pregnancy and delivery is postpartum hemorrhage. Bleeding disorders are associated with an increased risk of bleeding, both immediately after and for several weeks following delivery. Women with platelet function disorders should therefore work with their doctors (both bleeding disorder specialist and the obstetrician) to develop an individual delivery plan. This plan should address all stages of labour, including delivery of the placenta, to reduce the risk and severity of bleeding. Treatment is different for each woman and depends on her personal and family history of bleeding symptoms, the diagnosis and severity of the inherited platelet function disorder, and the mode of delivery. Women with platelet function disorders should be advised to contact their health care provider immediately if postpartum bleeding is excessive.
In some circumstances, infants born to women with inherited platelet function disorders may also be at risk of inheriting the disorder and experience bleeding. Difficult and prolonged labour, and deliveries that require instrumentation, such as the use of forceps or vacuum extraction, should be avoided.
Learning that you or a family member has an inherited platelet function disorder can be upsetting and you may experience a range of different emotions. For some people, it may cause fear and anxiety, while for others, being able to put a name to the symptoms that they have been experiencing can be a tremendous relief. Parents may feel guilty to learn that their child has inherited a genetic disorder. All these feelings are normal and are likely to change over time as you learn more about the condition and the impact it will have on you or your family member’s life.
Talking to others—friends, parents, health care professionals, and other people with inherited platelet function disorders—can be comforting. Learning as much as you can about the disorder will help you feel more confident and relieve your fears. Get in touch with your local patient organization or bleeding disorder treatment centre to ask questions and discuss options. Patient groups and treatment centres can be located through the WFH website at wfh.org/find-local-support/.
People with inherited platelet function disorders should be followed by a treatment centre that specializes in the diagnosis and treatment of bleeding disorders, as they are most likely to offer the best care and information.
A healthy diet and regular exercise keep the body healthy and strong. Exercise can also help reduce stress, anxiety, and depression, and reduce the frequency and severity of bleeding events.
Some food or food additives, such as alcohol, fish oils, Chinese black tree fungus, ajoene (a component of garlic), and several herbal remedies, may affect platelet function and make symptoms worse.
Good oral hygiene is essential to prevent tooth decay and gum disease. For people with inherited platelet function disorders, maintaining good dental health is very important to reduce the need for dental surgery, which can be complicated by excessive or prolonged gum bleeding. People with platelet function disorders should:
Invasive procedures, such as scaling, extractions, or root canals, may cause bleeding in people with platelet function disorders. The dentist should consult with the bleeding disorder treatment centre to determine the individual’s potential risk and to develop an appropriate plan to prevent or treat bleeding for any procedure. Medications may be needed before the procedure to prevent bleeding and ensure an uncomplicated procedure and recovery.
People with platelet function disorders should be vaccinated. Vaccines may need to be given subcutaneously (under the skin) rather than directly into the muscle to avoid the associated risk of bleeding, and this should be discussed with the clinician who looks after the platelet disorder.
Check with your doctor before taking herbal remedies or medications. Some over-the-counter medications, such as aspirin (acetylsalicylic acid) or other nonsteroidal anti-inflammatory drugs (such as ibuprofen and naproxen), should be avoided as they interfere with platelet function. Many other drugs can also affect platelet function, including blood thinners (anticoagulants), some antibiotics, heart drugs, antidepressants, anesthetics, and antihistamines. Medications that interfere with platelet function should not be used without specific medical advice from a doctor familiar with your platelet disorder.
People with bleeding disorders should always carry information about their disorder, the treatment required, and the name and telephone number of their physician or treatment centre. In emergencies, a medical alert bracelet or other identification, such as the WFH International Medical Card, notifies health care personnel of your inherited platelet function disorder. Before traveling, find the address and telephone number of the bleeding disorder treatment centres at your destination(s) and take this information with you in case you need care. Treatment centres can be located on the WFH website (wfh.org/find-local-support/).